Postpartum Complications: Who’s At Risk?
Postpartum is a time to heal and relish in being a new mother, but transitioning into this new phase of motherhood isn’t always without its complications.Postpartum is a time to heal and relish in being a new mother, but transitioning into this new phase of motherhood isn’t always without its complications. In this article, we will outline who’s at risk for postpartum complications as well as the signs to look out for and preventative measures to integrate to reduce or eliminate risk factors.
Who’s At Risk?
The postpartum period where most complications manifest is in the first six weeks after childbirth. Postpartum complications are increasing, and so remain a concern for all mothers. The CDC (Centre for Disease Control and prevention) claims that 3 out of every 5 pregnancy-related deaths can be avoided with early detection and treatment in the US. Not all postpartum complications are physical by nature. Emotional and mental stability are considered part of the range of postpartum afflictions.
Some pregnant women will exhibit major depression symptoms during their pregnancy, or it will begin in the first month after delivery. This is known as “peripartum depression.” Postpartum depression is depression that begins within the first month after delivery. In both cases, the condition is major depression, but the timeframe stems from pregnancy to the first four (4) weeks after delivery.
Strangely enough, postpartum complications affect women after childbirth, but there are reported cases of men (husbands) suffering from some postpartum symptoms. These include fatigue and changes in sleeping and eating patterns. An estimated 4% of fathers experience some form of depression in the first year after the birth of their child. If there is a history of depression or if there are financial constraints or difficulties, the risk of depression increases. Before we dive deeper, let’s talk about baby blues.
Baby Blues
We covered Baby Blues in depth here and here. In summary, the phrase “you’ve got the baby blues” is commonly associated with new mothers shortly after childbirth. About 70% of all mothers experience the baby blues directly after childbirth, primarily due to a change in hormones combined with stress related to isolation, sleep deprivation, and fatigue.
Mothers will feel emotionally overwhelmed and will be tearful for no particular reason. The baby blues will become noticeable a few days after delivery and will peak in the first week, then slowly subside in the second week. This is an adjustment period where mothers learn to cope with their physical, emotional, and mental changes.
It’s important to note that having the baby blues is not considered a postpartum complication. Although the symptoms are similar or included as part of postpartum complications, they are considered normal and dissipate on their own within a few weeks. Never-the-less, mothers should be given all the necessary support to help them adjust to their changed lifestyle.
The Risks of Peripartum & Postpartum Complications
Peripartum symptoms during pregnancy can influence a mother’s health. This will directly affect her unborn child’s growth and development. In some cases, severe symptoms can lead to premature birth and will negatively affect the necessary early bonding between mother and child.
If left untreated, postpartum complications can lead to death. Research indicates that more than half of all pregnancy-related deaths occur after childbirth. The CDC listed the most common causes of pregnancy-related deaths as follows:
- Cardiovascular diseases, including cardiomyopathy
- Underlying or pre-existing health conditions
- Infection or sepsis
- Excessive bleeding after childbirth
- Blood clots that travel from the legs to the lungs (Thrombotic pulmonary embolism)
- Stroke
- High blood pressure
- Amniotic fluid embolism is a rare condition when fetal cells enter the mother’s bloodstream.
- Anaesthesia complications.
It is not always possible to pinpoint the exact cause of pregnancy-related death. However, the risk of death related to pregnancy complications is very low, but women who suffer from obesity, cardiac diseases, or high blood pressure are at greater risk.
Signs and Symptoms
Postpartum complications are treatable, and the earlier treatment begins, the better for your health and that of your baby. Here are some warning signs and symptoms that will require immediate medical attention:
- Chest pain
- Problems with breathing (shortness of breath)
- Seizures
- Thoughts of hurting either yourself or your baby.
- Excessive vaginal bleeding with large blood clots
- Infections, urinary tract, and uterus
- An incision that isn’t healing
- One of your legs is swollen, red, painful, and warm to the touch.
- A fever
- A constant headache with vision changes.
- Rapid heartbeat or heart palpitations
- Mastitis
- Perineal, vaginal, breast and C-section incision pain.
- Foul-smelling vaginal discharge
Prevention
The baby blues are common among new mothers and are not reflections of poor health or being inadequate in any way. Pregnancy, labor, and childbirth can be very traumatic, not to mention the changes occurring in your body linked to hormone changes. All this can be overbearing for most new mothers faced with taking care of a new fragile life. Fatigue sets in pretty quickly, and it can unleash a torrent of emotions that have you crying out for a bit of help. Here are pointers that may help prevent any serious peripartum or postpartum complication:
- Stay healthy during your pregnancy and do not smoke or use any drugs without your doctor’s knowledge.
- Do light exercises like yoga that have breathing exercise components.
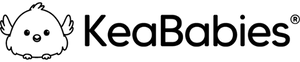
- Prepare for the arrival of your baby. Have enough diapers, clothes, bottles, and other items you will need to take good care of your little one.
- Create a support circle of family and friends who can help look after your little one while you get some much-needed rest.
- Take good care of your personal hygiene and monitor your recovery.
- Schedule an immediate appointment with your doctor if you notice any of the symptoms discussed above.
- Once you leave the hospital, set up an appointment with your doctor for a check-up two or three weeks from your discharge date.
- Don’t try and go it alone. Accept help, and don’t be afraid or embarrassed to say you are not coping. Be transparent about how you feel so the people around you can help out if need be.
Conclusion
If any serious issues arise, such as chest pains, fainting, or uncontrollable bleeding, notify your doctor immediately. If necessary, go to the hospital emergency room for an examination and possible treatment. KeaBabies can provide some assistance with our simple to use but precise, dependable, and clinically approved blood pressure monitors.
Take good care of your health, and know that there are always good people willing to help no matter your circumstances. Your good health will filter down to your baby, and you will be rewarded with much happiness.
|
|
Meet Our KeaMommy Contributor: Nadia Rumbolt Nadia Rumbolt is a mom of many trades, including creative writing, blogging, van life, minimalism, veganism, the beach, nature, and the occult. |